Music therapy: the art of healing through music
From ancient temples to modern hospitals, music has always been part of healthcare. Far from being just entertainment, music therapy is a therapeutic discipline in its own right. Emmanuelle Karrer has been working for nearly twenty years in psychiatric wards and retirement homes as a music therapist, sound therapist and addiction specialist at emeis, using alternative methods to heal patients.
Since the dawn of time...
The French Federation of Music Therapists defines music therapy as a practice that uses sound and music to restore or support communication, expression and relationships, both verbally and non-verbally.
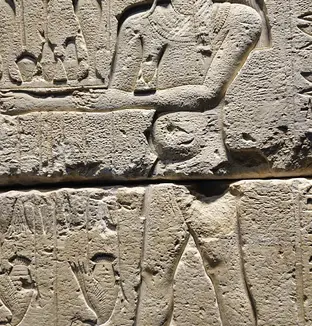
In ancient times, the Egyptians already used music in their healing rituals. Aristotle emphasised its soothing virtues, Plato its influence on the soul. In medieval Italy, doctors made people bitten by tarantulas dance until they were exhausted to "drive out the venom," giving rise to the tarantella, conceived as a therapeutic dance.
The professionalisation of music therapy began in the 20th century, particularly in American military hospitals in the 1940s, where musicians worked with traumatised veterans. In France, Jacques Jost founded the first national music therapy centre in 1972. Since then, the practice has developed widely in healthcare and medical-social facilities.
When music soothes the soul
Chronic pain, anxiety or depression, addiction, language disorders, neurodegenerative diseases, autism, oncology or end-of-life care: music therapy is used for all ages, including in neonatology.
Its effects are now well known:
- Reduction of pain and anxiety
- Regulation of heart rate
- Stimulation of memory and attention
- Improved motor skills and language
- Reduction of agitation in patients with neurodegenerative diseases
"Some patients with Parkinson's disease stop shaking during the session," says Emmanuelle Karrer. "I've also seen two teenagers resolve a conflict by turning it into a rap battle."
For Emmanuelle Karrer, music is an essential tool, including for her patients suffering from addiction: "Addiction is an emotional illness: the substance is used to numb or exacerbate emotions."
With mental health, music often becomes the indirect way in which patients dare to talk about themselves. But the role of the music therapist is essential in the process: it is not the music that heals in the long term, but rather the listening and approach of a trained professional. Music allows patients to put their emotions into words. "You can't regulate an emotion you can't identify," the practitioner reminds us.

A personalised therapeutic approach
Each course of treatment begins with an individual assessment. Emmanuelle Karrer explores the memories associated with music, physical reactions, and cognitive and motor skills. This preliminary work guides the choice between two complementary approaches: on the one hand, active music therapy based on sound production, and on the other, receptive music therapy based on guided listening.
Sessions can be individual or group sessions (between six and eight people). Individual formats are preferred when the patient's mental state does not yet allow for group work. The tools used are deliberately accessible to all: intuitive percussion, voice, breathing, wordless singing, movement, relaxation, writing or drawing under musical induction. Emmanuelle Karrer emphasises: "This is not a music class. Musicians sometimes find it difficult to accept that it's cacophonous... The aim is not to 'play well', but on the contrary, to let go." During these sessions, some patients write songs, draw or dance freely while listening to melodies chosen by the specialist or the participants. "The aim is to allow everyone to express themselves," explains Emmanuelle Karrer.

The crucial role of carers
But music therapy is not just about the patient: it affects their entire environment. In nursing homes, relatives provide information about musical tastes, important memories and songs that have accompanied the resident's life. This information becomes a therapeutic tool, and carers sometimes even participate in the sessions.
Emmanuelle Karrer recalls an aphasic woman who had been silent for months, to whom she hummed a famous nursery rhyme. The patient listened, then turned to her husband and whispered the end of the chorus. A moment suspended in time, made possible by music therapy.
More than ever, there is no single approach to care, no single way of treating patients. At emeis, multidisciplinarity is the watchword: since each person is unique, so is each journey... sometimes to music!

